Certain patients with an aggressive form of ovarian cancer have a better chance of a cure through surgical removal of their tumor before chemotherapy instead of the reverse, a new study shows.
Led by researchers at NYU Grossman School of Medicine, Perlmutter Cancer Center, and Dana-Farber Cancer Institute, the study used a mathematical tool to examine how doctors should coordinate available treatments for high-grade serous ovarian cancer (HGSC).
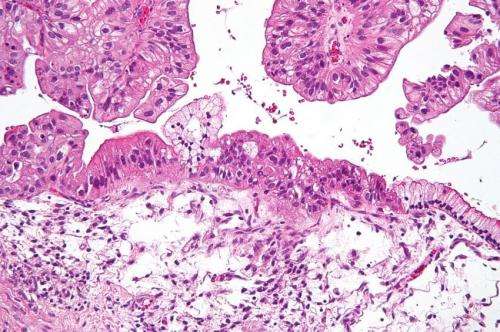
Ovarian cancer is the 8th most common cancer and cancer death in women worldwide, and HGSC constitutes roughly 70 percent of ovarian malignancies and has the worst prognosis. Patients with the condition typically undergo surgery and chemotherapy, but there has been long-standing controversy over the best order of treatment.
Published online June 14 in Proceedings of the National Academy of Sciences, the new analysis argues that patients who can undergo “complete debulking” surgery first, with chemotherapy added after (termed primary debulking surgery or PDS), should have a superior outcome to the other main treatment option: giving patients a few cycles of chemotherapy to shrink the tumor before surgery (neoadjuvant chemotherapy or NACT).
“The issue of whether PDS or NACT should be used was highly controversial, and a major reason for it lies in the different characteristics of patients in different clinical studies,” says study first author Shengqing Gu, Ph.D., a graduate from University of Toronto and now an instructor at Dana-Farber Cancer Institute. “We therefore built a mathematical model to simulate HGSC clinical course, which allows us to compare treatment outcomes in the same virtual patients and examine which group of patients may respond differently to PDS vs NACT.”
“Our model, combined with earlier clinical data, suggests that for patients who can undergo complete debulking, surgery offers the best chance of long term survival or even cure,” says study co-senior author Benjamin G. Neel, MD, Ph.D., director of Perlmutter Cancer Center at NYU Langone Health. “Our model also provides some insight about optimal early detection and treatment intervals.”
The researchers used clinical data from roughly 300 patients in previous studies of patients’ responses to PDS or NACT, taken from the Princess Margaret Cancer Center in Toronto and the Canadian Cancer Trials Group.
The researchers found that in patients who are well enough for surgery, debulking provides better results because it has the best chance of removing cancer cells resistant to chemotherapy. For patients who are too ill for debulking surgery, the study suggests that a shorter period of initial chemotherapy, rather than the currently recommended interval, might provide a greater benefit.
The current analyses suggest several questions that future randomized clinical trials should examine, say the study authors. These include how much the influence of the time gap between surgery and subsequent chemotherapy may affect treatment outcome, whether there is a link between the number of initial chemotherapy cycles and outcomes, and whether complete secondary surgery on relapsed tumor improves prognosis.
Source: Read Full Article