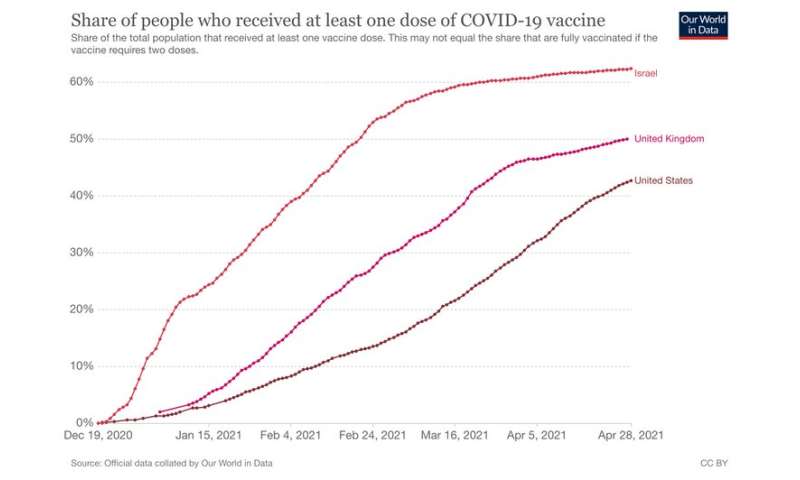
Now that Britain and the US are crossing the 50% threshold of their populations vaccinated with the first dose, are they reaching herd immunity and can things return to normal soon?
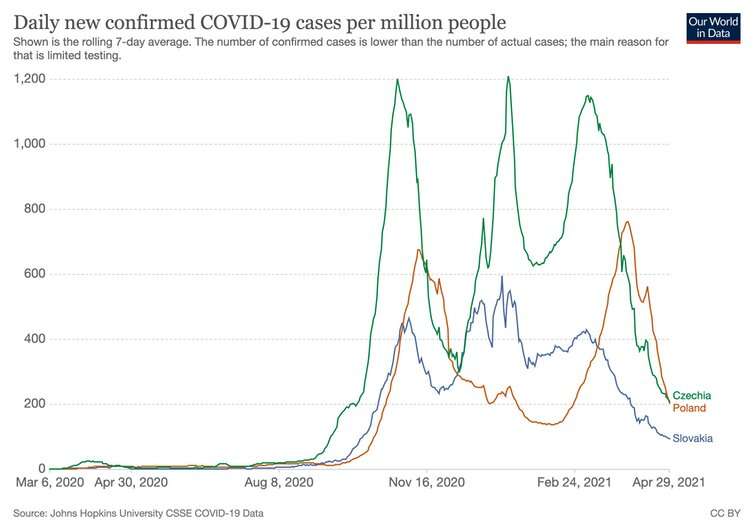
Not yet, is the short answer. And focusing on a single number is not helpful. It might encourage behaviour that would lead to another wave breaking out, such as relaxing social distancing or—on the government’s part—opening borders. Indeed, countries such as the Czech Republic, Poland and Slovakia experienced relatively small first waves, but a massive second outbreak.
India is particularly concerning. Last year, some researchers and politicians claimed that cities such as Mumbai, Delhi and Chennai might have reached herd immunity. Yet following a relaxation in control measures and border controls, India and Nepal are currently experiencing a devastating second wave.
So is the UK close to the point at which things can go back to normal? The vaccination drive has been amazingly successful; cases are down and, more importantly, hospitalisation and deaths are down. A recent study shows that the vaccine is successful not only in protecting people from becoming seriously ill but also in significantly reducing transmission. There is now a window of opportunity to eliminate the virus in the UK, or at least to bring it to near extinction, and to concentrate on controlling isolated outbreaks.
The most common estimates for the herd-immunity threshold for the original coronavirus strain—the so-called wild type—are at 70% or more immunity. For the new variants, the threshold is probably higher. Also, we know that vaccines have limited effectiveness, which further increases the proportion of the population that needs to be treated.

It is important to note, too, that there are pockets of the population where vaccination level is lower than the national average. These pockets are potentially a breeding ground for super-spreading events. These sorts of outbreaks, although initially small, can lead to the establishment and subsequent spread of highly infectious variants. The danger is well illustrated by the spread of the Brazil variant in Canada or the UK variant in Europe.
With infection levels still very high globally (the number of new infections is higher now than it ever was last year) there is significant potential for new variants to emerge. Although it looks as though the mRNA vaccines (Pfizer and Moderna) are effective against the new variants, the “variant of interest” in India may be more problematic.
Finally, in many countries, a significant proportion of people is unwilling or unable to be vaccinated or to take precautions against infection. The vaccination levels needed to cross the line might not be achievable at all, even in the long term.
Vaccination levels, even in places like Israel where 62.4% of the population has been vaccinated, are still not high enough to fully protect against future outbreaks while relaxing all regulations. The government in Israel has lifted most—but crucially not all—internal regulations. The borders are, however, still closed to non-essential travel and masks are still worn indoors. Schools only reopened at 57% vaccination level.
Not safe until everybody is safe
As long as the virus is not eradicated everywhere in the world, there will always be a danger of the rise and spread of new variants. Rather than focusing on whether we reached 70%-80% of the population—and the UK is not there yet—it is more useful to think of herd immunity as a process of virus suppression and elimination. However, this strategy does not necessarily mean experiencing high infection numbers or strict lockdowns.
Having driven the numbers down, the government will need to continue to keep a combination of control measures in place. They will be applied at a low level and hopefully much less intrusive than the current ones. The strategy will include a continuing vaccination drive with re-vaccination in response to new variants. Masks will continue to be worn in places where the risk of infection is high.
There will still need to be an intensive regime of tests. False negatives (where the test says you don’t have the disease when you actually do have it) are of particular concern, as they can make people less careful and so can lead to outbreaks. But false positives (where the test says you have the disease, but you don’t) will also need to be followed up with the more accurate PCR tests, as having too many false alarms can lead to people avoiding the procedure. Border controls such as COVID tests and vaccine passports—but hopefully not a travel ban—will help to keep the outbreaks to the minimum.
Source: Read Full Article