
Last night, the federal government announced substantially revised plans for the use of the AstraZeneca vaccine in Australia.
Due to concerns about the vaccine’s possible links to a rare blood-clotting disorder, and following advice from the Australian Technical Advisory Group on Immunization (ATAGI), the Pfizer vaccine is now preferred for people under 50.
These developments raise questions about how authorities and individuals assess risk, and respond. Let’s try to make some sense of it.
What’s happened?
Reports about rare blood clots possibly associated with the AstraZeneca vaccine have been floating around for a few weeks now.
So why has it taken so long for the government to clarify this relationship and make the recommendations? Authorities haven’t been keeping us in the dark.
When you have a new condition like this, and experts are examining data in real time, it takes a while to understand exactly what’s going on: to develop a clear case definition, to be confident what you’re seeing is a real phenomenon, and importantly, whether it’s likely to be caused by something in particular (in this case, the vaccine). It’s made more difficult when the event is very rare.
After reviewing a wide range of data relating to cases of this rare blood-clotting syndrome predominantly in the United Kingdom and Europe, Australian experts have now reached the threshold of evidence they needed to be satisfied there may well be a causal link between the AstraZeneca vaccine and this condition.
Understanding risk
It’s important to note every therapeutic agent (a drug or a vaccine, for example) carries the risk of unintended consequences. For most of us, most of the time, this will be minimal. This is a biological reality reflecting the interconnectedness and complexity of the human body.
So like for any other therapeutic agents, there are risks as well as benefits we have to accept in taking COVID vaccines. What we need to do is to weigh up these risks against the benefits.
We make these sorts of calculations every day in all aspects of our lives. When we decide to get in the car, we know there’s a risk associated with driving. But we assess the risks are worth taking as the benefits of getting where we want to go quickly are worth it.
Mostly, we make these calculations without being consciously aware we’re doing it. Sometimes the parameters underlying these calculations are easy to grapple with—but sometimes they’re more nebulous.
Weighing up the risks and benefits of the AstraZeneca vaccine
We know the vaccine offers near-complete protection against severe disease and death from COVID-19.
We also know severe side effects from the vaccine, in particular vaccine induced prothrombotic immune thrombocytopenia (VIPIT, the blood-clotting disorder in question), are extremely rare. But the condition is serious and around 25% of people have died after developing VIPIT.
There are a range of estimates of how often this syndrome occurs. But it’s generally accepted its incidence is about 4-6 cases per million doses of vaccine.
To put it in perspective, this puts the risk in the same order of magnitude to the average risk of dying if you complete a marathon, go scuba diving, or rock climbing.
It’s also important to note that we’ve started to see a pattern in that those who are at higher risk of this syndrome tend to be younger and tend to be women. We don’t have a clear understanding of why this is, but recognizing this is really helpful in terms of making decisions about how to mitigate this risk.
Why the balancing act isn’t so easy
Although we have a pretty good understanding of the rate of severe outcomes from COVID-19, since we have over 12 months’ experience now of this illness, context is important. There are different levels of risk depending on where you live and what the rate of transmission in the community is.
While it’s all well and good in some countries to say you’re more likely to get very sick with or die from COVID than experience a complication from the vaccine, in Australia we have next to no COVID, so the risk of adverse outcomes from COVID is much lower. This needs to be factored into the equation.
We also have different strains of the virus, which can vary in how infectious they are and how sick they might make you. This also needs to be added to the mix.
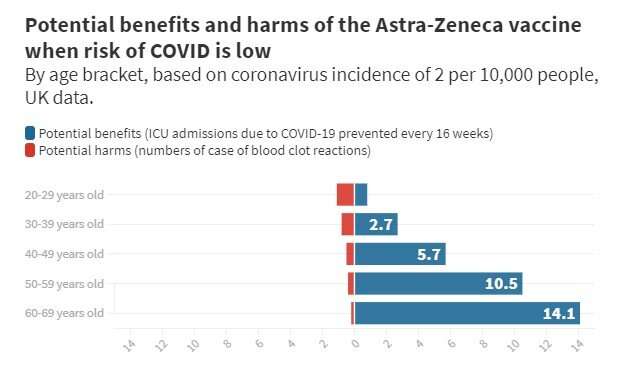
In acknowledging the difficulty in completing these risk-benefit analyses, it’s really helpful to use a visualization the University of Cambridge has put together based on UK data, which we’ve adapted here, comparing the risks and benefits of the AstraZeneca vaccine.
It depicts the risk of adverse effects from COVID (being in ICU) against adverse outcomes from the vaccine, based on an assumed incidence of COVID in the community of two in 10,000 people. Although the incidence rate in Australia is lower than this, this visual is extremely useful in conveying the nature of the relationship between the risks and benefits of the AstraZeneca vaccine in Australia.
What this visual shows clearly is that the benefits of the vaccine increase the older you are, because the risk of severe disease is higher the older you get.
It also shows that although the risks of side effects from the vaccine are relatively small regardless of age, the gap between risks and benefits narrows the younger you are. This is in part due to the reduced benefit of the vaccine for younger people who are less likely to have severe symptoms from COVID, and in part due to the increased risk of serious side effects, such as blood clots, for younger adults.
Source: Read Full Article