According to the American Journal of Roentgenology (AJR), antithrombotic therapy was not linked to increased incidence of traumatic intracranial hemorrhage on CT in adult patients, although the therapy did show association with hematoma expansion at follow-up.
“The findings suggest, in patients with good neurological status after ground-level fall, application of a similar strategy for selecting patients for initial head CT, regardless of antithrombotic therapy use,” wrote first author Zeynep Vardar at the University of Massachusetts Medical Center in Worcester. “If initial head CT shows traumatic intracranial hemorrhage, early follow-up head CT should be systematically performed in those on antithrombotic therapy though possibly deferred in other patients.”
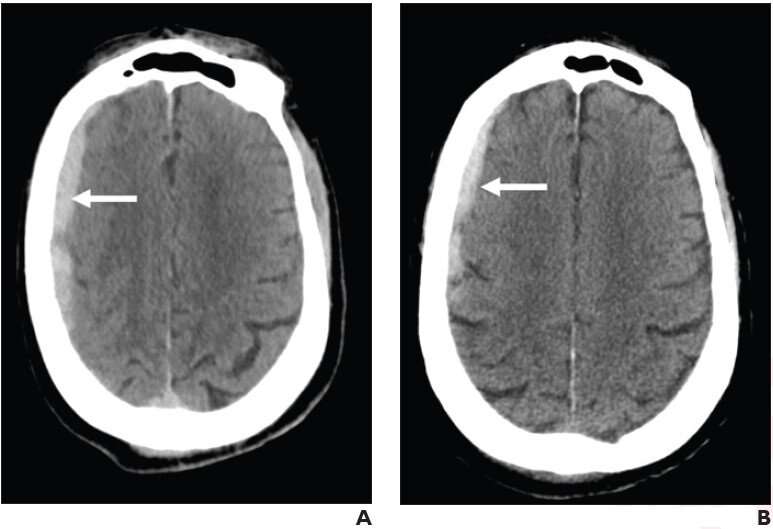
Vardar and colleagues’ retrospective case-control study included 1,630 patients (693 female, 937 male; mean age, 80 years) who underwent head CT after presenting to the emergency department (ED) with ground-level fall (Glasgow Coma Scale ≥ 14 and no focal neurological deficit) between January 1 and December 31, 2020. Initial head CT examinations were reviewed for traumatic intracranial hemorrhage characteristics and follow-up head CT examinations (performed within 24 hours) were reviewed for hematoma expansion, with clinical outcomes extracted from medical records.
The frequency of intracranial hemorrhage after ground-level fall with good neurological status was not significantly different between patients on antithrombotic therapy and those not on antithrombotic therapy (4.4% vs 3.1% respectively, p = .24). However, hematoma expansion occurred more frequently in patients on antithrombotic therapy (26.2% vs 4.8%, p = .04).
Source: Read Full Article